When Words Fade: How Activities Spark Connection in Dementia with Sharon Daltry - Ep 81

Welcome to Caregiver Relief Podcast, the show where we explore real world strategies, stories, and support for family caregivers and professionals carry for those with dementia.
I'm Diane Carbo, RN and founder of Caregiver Relief. Today we're shining a light on one of the most overlooked yet powerful approaches in dementia care, the role of activities in fostering calm, dignity, and connection, especially in the later stages of the disease. So often, we focus on medications for managing behaviors, but what if the real key lies in meaningful engagement?
Our guest knows this firsthand, and I'm honored to welcome Sharon Daltry, co -founder and director of TimelessPresents. A UK -based social enterprise creating dementia inclusive activities that help families and care teams reconnect with their loved ones. Inspired by her father's journey with Alzheimer's, Sharon has dedicated her work to developing tools that reach beyond memory loss and create those treasured moments of spark and recognition even when language and cognition have faded.
Timeless Presents has thoughtful products are now stocked by the Alzheimer's Society and a U .S. Public Service Announcements featuring the brand will be launching soon, a testament to how impactful this work truly is. In our conversation today,we'll explore how the right kind of activity can reduce stress, prevent challenging behaviors, and restore connection.

Sharon, thank you so much for taking time out of your busy day to share this
important information on timeless presence. Activities are one of the most overlooked approaches to care, yet is one of the most important things family caregivers and professionals overlook. So welcome and please tell me a little bit about yourself.
Thank you very much. I am co -founder of Timeless Presents. My dad had Alzheimer's for 17 years and over that period we had him at each stage
for a significant amount of time. I'm a communicator, he was a communicator and we managed to stay connected until the very end stages. Like most people,
I found myself floundering. I didn't know how to connect with him and it was
painful. It was painful for me and it was confusing and upsetting for him.
Basically because of the realization that we needed to interact with him differently
in this stage, then we managed to maintain connection. And the things that we understood after he passed in 2019, and there was a period of grieving obviously, but then when I looked for the products that I knew must exist by now, because we're talking, he was diagnosed in 2002.
We're talking a very long time ago and they just still weren't there. So my husband and I, decided that we would share what we had learned in this situation by producing products that were inclusive for people with dementia.
So what makes dementia inclusive activity different from from something simply labeled dementia friendly?
Well, what we have done is we have designed our products from the ground
up. So we did the research about not only dementia, but all of the other core orbit
conditions, visual problems, cognitive problems, those kinds of things.
And we have built and designed from the ground up to make sure that we are lowering the barrier to entry. This is so that as many people as possible can interact with our products.
It's designed for one purpose and that's for activity in late -stage
dementia.
Why do you think late -stage dementia care, especially around engagement,
is so often overlooked? And how can we start to change that?
There's a huge stigma still. I think there are various elements to this. There is
stigma around dementia. And when they go into the later stages, they quite often become nonverbal, very hard to engage. That's when challenging behaviors can start to manifest themselves. I also think, having been through the journey myself, there is, you decide, I've done a lot, I've already done so much and there's a little bit of relief there, but somehow somebody gave you permission to stop trying, and it's too easy to lean into that.
I didn't quit trying. My husband didn't quit trying. I think and the
thing is, it's essentially flipping everything on its head. At this point you
want, you need to do is give it a go. It doesn't matter if it's imaginary it doesn't matter if they don't understand. It matters that they feel safe and supported And it means to try and observe the world, from their point of view.
I love that. And you know what, one of the things that you are offering us, as so
many other caregivers that have been through their experience, is you're sharing what you've learned about your journey and created a solution to a problem. Nothing is more challenging than the late stage dementia behaviors.
It's so hard for so many people, for caregivers, they are expected to do so
much and they have no idea. So that's why I'm really excited about letting the
world know what you've created. It's just, we're benefiting from your caregiving
journey and I appreciate, I want to thank you, because you're going to
make other people's life easier that are caring for someone at home.I really like that. So thank you.
Sharon, how can families or care partners use these tools or approaches without meeting specialist training?
What we've done, I don't know what the situation is like in the US, but in the
the UK, the figure for carers actually working in care homes, 70 % have received no
dementia training.
It's the same here, it's the same here. And I find this particularly shocking.
So what we have done is, apart from the design principles that we have included in our products, what we have done is we've come up with five hints and tips that come with every single product. So anybody can pick up a product and they have got hints and tips attached to it that they will be able to use to start having a meaningful interaction with somebody who has dementia.
That's the idea. I broke it down to as few pointers as I possibly could.
And the first one is to commit to participating because this is not just product,
this is product and this is ethos. You have to commit to doing this and engaging
and spending time with them so that they know that you're there for them.
One of the things I find when caregivers get to, the family caregivers get to the
late stages, they feel tired, they feel overwhelmed. And I love that you've already
addressed, they need to commit. That's really hard for many of them.
But I take a care team partner approach and I encourage my clients to follow that
approach where, you know, if you have someone that can help you with other things so that you can enjoy time with your loved one while you're providing care.
That's more important than getting the cleaning done, the laundry done or whatever.
Ask somebody to help you with those things because you're losing your person slowly over time and those moments of spark, that glimmer where you connect are priceless..
I love And I love when you know you've connected with your loved one and you
never know if it's going to happen again or not. But the commitment to creating
these opportunities is what makes it special.
It's where it all starts. I'm here for you. This is our time.
I love that, I really love that.
So we know that activities can help prevent or reduce challenging behaviors, but can you share some examples how engagement has eased the stress in advanced care settings? -
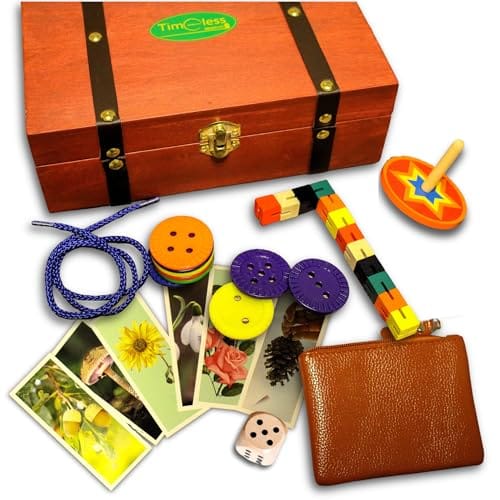
Not specifically advanced care settings. I can, 'cause we have something called a curiosity box. People mistake it for a memory box, which it isn't.
My dad had something similar and it allowed us to be able to take him places. I
could even very late on. I could take him for a cup of coffee to a coffee shop
and we would sit there. Then, he would point he would wanted to go home. This was fairly early on he would notice the box, he would investigate it,
he would take everything out of it,
See if everything went together. And then he would come back to the conversation. It would kind of reset him to, okay, I'm here. Now there are people talking, and oh, I can join in a little bit with this conversation.
I love that you can take him out because socialization. People don't understand that is such a key to slowing the process of the disease and also giving the caregiver ability to be out and about for a while and enjoy their loved one as well.
Absolutely, and it just came naturally to me to try and do it,. I was lucky enough to find a way to enable that. I just remembered actually, we visited a care home, and there was a gentleman there who was introduced to our puzzle. He's actually the one in the video and the actual activities coordinator came up to us and said to her that he had said it was brilliant. It was the first time he had spoken in six weeks.
Oh, oh, that's powerful. Wow. It is because what we're doing is we're making things that they can interact with that they want to interact with.
We're designing them based on children's toys, puzzles, that kind of thing. However, they are all adapted to look dignified adult.
I love that you're doing it because one of the things that caregivers have a
hard time with or and some of the patients themselves, those suffering from dementia, don't want, to look as if they are playing with baby toys. They may feel insulted by that. Some of them, not many, but it does happen. I like that, you've made them so that, they are able to relate so much too.
That was the plan and it seems to work. It seems to be, I think also there is
this reluctance because I think their self -esteem as they go through the journey
takes a battering. I really do. I think they are afraid to try.
Many of them lose their ability to be motivated to initiate something and that
starts early on in a lot of dementias depending on the type. So when you get to
the late stage You're right. They've been beaten up in their minds, they're unsure,
they're uncomfortable, and sometimes things aren't making sense to them.
I love that your products, like the Curiosity Box has me very curious. I
think that's an awesome tool. It has a tool e it keeps them busy.
If you're giving them an opportunity to interact or to focus on something and use their hands, in a safe environment, it's really, they're connecting.
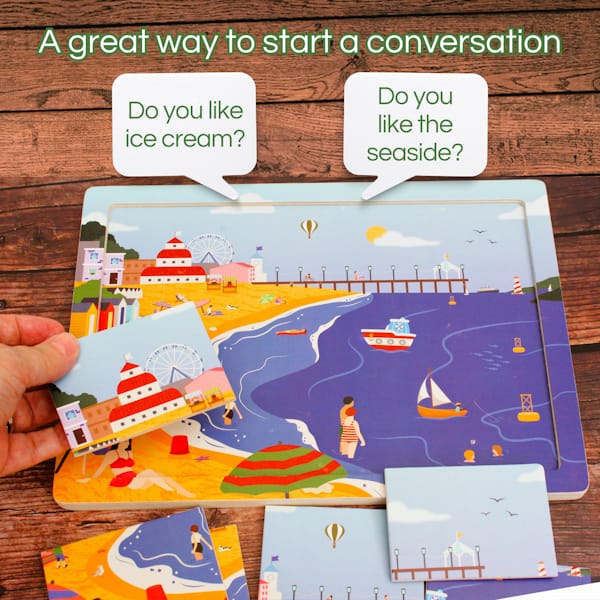
That's really important, I think. I think also what we have done with all of
our products is to try and move away from a target that there is a point to
everything. It's being in the moment that is important. important. So even our puzzle pieces, they're all square so it doesn't matter if they put them in wrong, they
will still fit. They get the enjoyment and the empowerment out of it,
then job done.
Exactly, exactly. I love that you that's a key principle of your products. People with dementia lack self -esteem. They become unsure. You're giving them an opportunity, you're setting them up for success and that's really important.
Tt's really, really important but it's a sea change for the whole community to think like that. This is where we are.
It absolutely is a sea change because people don't realize or don't expect. One of the things they don't understand is a a person with dementia has slow processing thinking, and they lack reasoning ability after a period of time. They may not understand what you are saying to them, but, they will understand how you are saying things to them.
They will feel your energy, whether it's frustration or joy or happiness. So, I think that when you're doing a project and you're experiencing something, providing them with something that's simple, it gives them joy. It also gives the caregiver, joy.
It does. All of the memories that I have from that later stage are based around
the activities that we did together, the joy, the after the fun and the time that
I got to spend with him, I benefited as much as he did.
You know what? That is one of the most important things. That's what keeps caregivers going, is knowing that their interaction, their ability to provide care is working and they're doing a good job and that's their reward is having that connection with their loved one and I think that's really important.
So tell me, if a family caregiver listening today wanted to introduce more meaningful activities at home, what simple tips or first steps would you recommend?
I would obviously recommend our own products. We are a small social enterprise and we are available online. We have product in the United States at www .timelesspresents.net. Just try the hints and tips that we have.
Just give you a simple way to enter their world and start understanding what it is
that will help them to meet you.
What are five tips that you give with every package? What are they?
Okay, so commit to participating. Give them all of your attention. Make sure that you are engaging with them. Make sure that you're watching them as well. So that you can see, observe their reactions to what's going on.
The second one is do communicate on an adult level offering praise and encouragement like you would an adult. This is going to be difficult in some instances for people, but if they want to actually participate then communicate with them on that adult level. Because they are still adults and they're aware of that. That's something that's really important.
The third one is avoid questions that ask for a specific answer, like, do you remember? Good. Good. Because, the trouble is ,that it's so hard to stop doing that.
It's how we build all of our relationships, our whole lives. It's touch points of
shared memories. Then when you stop being able to do that,you lack the language to do it.
What you have to do is you have to use the activity in front of you and say, "Do you like this picture?" And you can start a conversation. And memories sometimes are actually available to people. They're just not theirs to command any longer. So what you can do is you're looking at things.
You're talking about things in the moment, but you're not asking them to
remember. Because asking them to remember is setting them up to fail.
You mentioned setting them up to success, but if you're not careful, you can set them up to fail.
Yes. Most people don't understand that somebody with dementia,
they're losing their ability to look to the future. They're losing their long
-term memory. So they really, truly are living in the moment, especially in the late stages of dementia. People don't understand that.
That's why I love your approach. I think it's positive. I hope that it creates a sea change of how we approach our care of our loved ones with dementia in the mid and even later stages of dementia.
This is what we hope, sincerely.
The fourth is if possible to let them lead, follow where they lead. Whatever that they're doing with the puzzle pieces or the curiosity box, it doesn't matter. Because they are exhibiting inquisitiveness. because that doesn't seem to go, that those kinds of things, and the final thing is simply have fun. Have fun, try and have fun in the moment.
I have to tell you that it's probably one of the hardest things for caregivers to
do because they're so anxious and stressed out all the time. They don't
understand that their loved one with dementia is picking up on that. If they
would really focus on just enjoying the moment and having a fun,
truly fun and relax, it could be so much better for them.
And it really does eliminate very challenging behaviors.
Exactly, I think a lot of challenging behaviors. I'm doing air quotes here, I think they're misunderstood. This is a personal opinion but you know when they start looping stories or asking the same question again and again and again. It feels to me that what they're actually doing is , they're finding themselves in a confused state. They don't know who you are. They don't remember anything about before and what they are doing is, they're reaching out to you with a question or with a story that they can remember.
Something that is safe for them to tell you. It doesn't matter that they told you 10 times a day. For them it's the first time. I think but being I could have been there, because I've heard this 10 times today and And it's very hard to keep that out of your voice. But if you can show up and actually participate in that gift that they are giving you. See is as they are reaching out from behind their confusion. Trying to communicate. I think that's misunderstood. I think a lot of the behaviors are misunderstood.
You're very right about that. You have to look at the cues that your loved one's given you. Check to see if they're hungry, they're thirsty. Do they need to go to the bathroom? Are they in pain? Can approach them? I always tell my caregivers I've been a nurse for over 50 some years. I've done care professionally and personally with family members. I know about dementia. I can tell you they are in the moment. I want to mention to the caregivers out there , make sure you pay attention of the environment around you. Turn the TV off.
If you're going to put music on, put soft music on, nothing loud and
boisterous. Make sure that when you start the activity, you're focused on the activity. Make sure the environment around you is conducive to having good interaction with your loved one at the time.
I think that's really important. It's part of the commitment. Exactly.

Looking ahead,Sharon, what's your hope for how dementia care, especially activity -based engagement? How to you see dementia care evolving over the next five to 10 years? We have a silver tsunami coming.
Well I'm part of it. Dementia care, we are not doing enough in the UK and the US . Obviously things are better than they are in other parts of the world. I really do want to see a change throughout the whole world, that we welcome these people. They get ostracized. I don't even think that's too strong a word to use. They get ostracized from society. That's not fair. It's so much of us, and you are hard pressed to find somebody whose life hasn't been touched by dementia in some way.
Exactly. I will tell you that the family caregivers are also ostracized because
they're afraid to take their loved one out for whatever reason or it's too much
work for them. They have a very small world.
Their world becomes very isolated socially and many and many other ways.
There's limited interaction. That's why I love your concept because if we can
promote that kind of concept, it's going to make life easier. People will
want to support this movement when they see how good a person responds to this
approach.
Ss someone who's worked in behavioral health, when a person has
dementia, it can be really hard when they're out of control with behaviors.
I hate that we have that they want to medicate. Oftentimes it's as simple as just the environment. They may be bored. They're afraid. They're cold. They're wet. They may be in pain. If you address all those issues and they are not the reason for the challenging behavior, then it's boredom. They need something to still stimulate them. That's what's really cool about what you're doing.
I love that you set a patient up for success. That's really important and the caregivers too. It's a good interaction for themas well. It absolutely is. The whole, mindset changed one day.
I was taking my dad in the car and we turned into a road and it was spring.
All of the trees down the road were full of pink blossoms. He went,
"Look at all the flowers on the trees." I got to experience that moment with
him again.! I get goosebumps every time I tell you about it.
Those are the moments we live for. They call it "the long goodbye" for a reason.
It's a cruel disease. We have moments where we do connect. we see that
glimmer and spark in their eyes. That's the person that you know. Then in a
moment, its gone. There's that blank stare there again.
So, we are always hopeful that they're going to improve. They're going to get better. It gives us hope.
It's a disease that you can delay the progression with these types of
activities. You can improve your interaction with these types of activities to
decrease challenging negative behaviors. I think that's really important.
I think I changed what I hoped for in the sense that I hoped that I could make
him happy when I was there, that we could connect. And that was enough. I stopped looking for more than that. I wanted to make him feel safe. I wanted to make him feel happy. If I felt like I'd achieved that, that, then that was good.
Sharon, you touched on a point that is very important. So continue with that thought because I love that. It's a strange thing. I almost say I had to give up on the idea of my dad being my dad, in order to be able to continue to have wonderful time with him.
Interesting perspective. I appreciate that. I tried to take my needs out of the
equation. I tried to understand what his world was like.
Once you kind of do that, flip it on its head, if I was sitting somewhere and
I was confused and I didn't know what was going on and maybe I'd lash out too.
Maybe I don't know what I do.
You're right, they're in an unfamiliar surrounding or what they know. They always talk about they wanna go home, even though they are home. Many times. It's a feeling they are looking for. I think sometimes they're talking about a feeling of comfort, of safety, of feeling secure.
I really like the fact that you've taken it off, take yourself out of the equation and put it, be more conducive to thinking how your loved one may be feeling at the time. I think that's awesome. I think that's a really important tip that every caregiver with caring for somebody with dementia should consider.
Thank you. It feels like that there is a widespread misunderstanding that you slowly empty out as a person. That by the end ,you're gone and that's
not what happens . It's not linear like that. You don't ever empty out.
The last the last time I saw my dad, before he passed, he waved me bye bye and blew me a kiss . I don't know if he knew who I was. That's OK
It was wonderful. He again reached out to me from a place that I can only
imagine. So yes, it's about understanding that they aren't gone. If they're quiet,
it's because they don't know what to say. They don't feel safe to say anything and
beaten. Yes. They're afraid to try anymore. - Exactly.
That's what I think anyway, I'm sorry.
No, you know what? You are sharing from your personal experience and that's really important for people to understand that you've had an amazing experience and you're actually providing a solution to a problem. We have no limited solutions out there for.
So I love that you have this product and you're helping, you're sharing your
knowledge with those that have, are still or are starting on their dementia
care journey.
Sharon, this has been such a valuable section. Where can listeners go
to learn more about timeless presence and the wonderful work you're doing?
We have a website : Timelesspresents.net in the United States. Anywhere else in the world Timelesspresents.com. We have the products there but we also share some of the background and some of the things that I've shared today. I'm active on social media. There is a public service announcement due to be released in
the United States fairly shortly
Which will give more information about what we're doing. We were contacted
last year. So that's happening.
Awesome. I'm excited for you.
To my family caregivers out there, I want to remind
you, You are the most important part of the caregiving equation. Without you,
it all falls apart. So please practice self -care every day. Learn to be gentle with
yourself ,because you are worth it.
Our Resources section can help you find the information and tools that you need. We have courses, videos, checklists, guidebooks, cheat sheets, how-to guides and more.
You can get started by clicking on the link below. We know that taking care of a loved one is hard work, but with our help you can get the support that you need.
Click here to go to Resources Section now!