Understanding and Managing Sundown Syndrome: Navigating the Challenges of Evening-Time Dementia Symptoms
Explore the complexities of Sundown Syndrome, a condition affecting those with dementia, marked by increased evening confusion and agitation. Learn about its causes, symptoms, and strategies for effective management to improve the quality of life for patients and caregivers.

What Sundowning Means?
Sundown Syndrome, also known as "sundowning," is a complex and intriguing phenomenon observed in individuals with dementia, Alzheimer's disease, and other cognitive impairments. This condition is characterized by a notable increase in confusion, agitation, anxiety, and sometimes aggressive behavior that typically occurs during the late afternoon, evening, or night. The term "sundowning" reflects the timing of these symptoms, often coinciding with the sun setting.
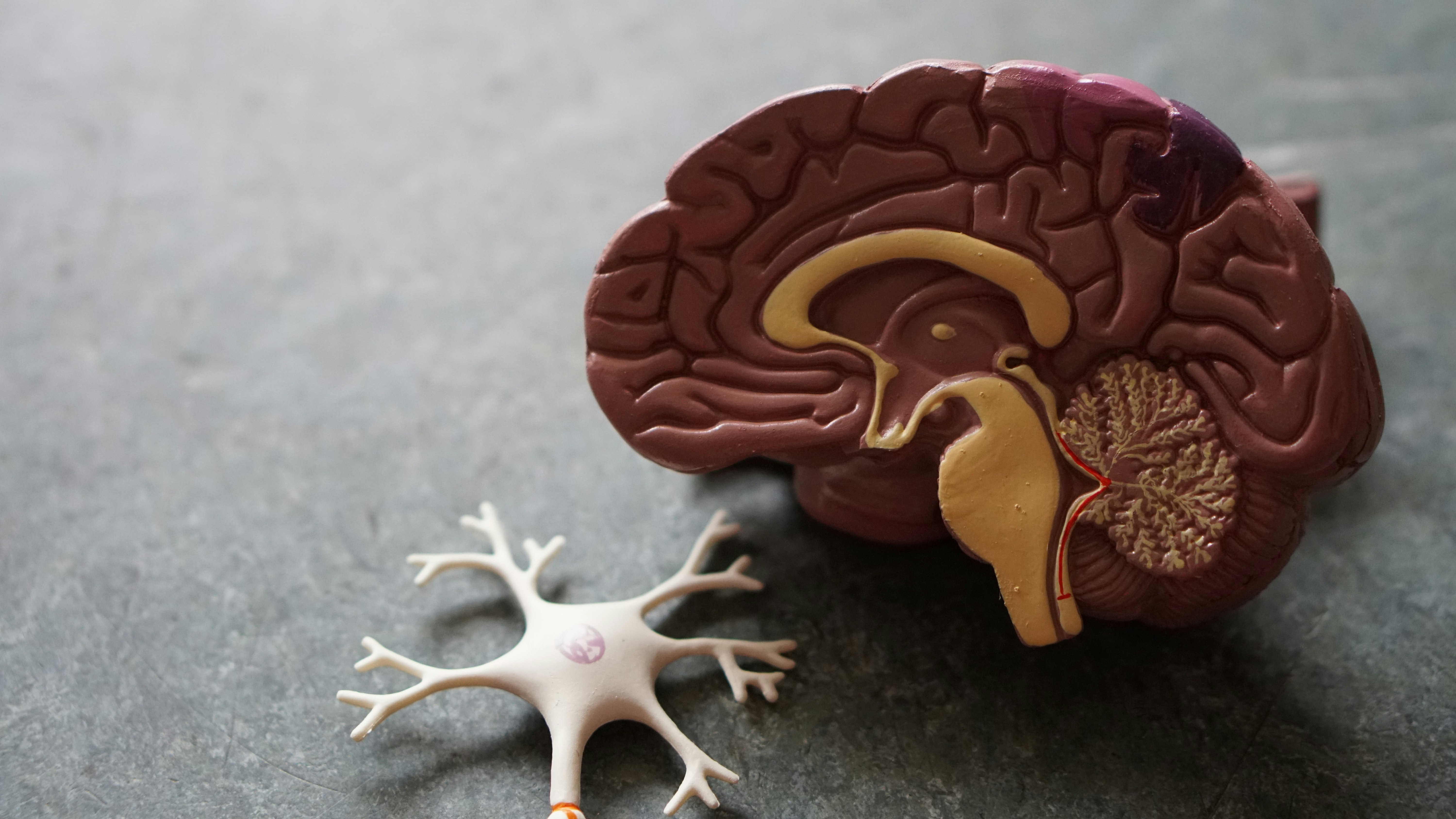
Understanding Sundown Syndrome
Sundown Syndrome affects a significant number of individuals with dementia and Alzheimer’s disease. While it's not a disease in itself, it is a group of symptoms that worsen in the later part of the day. This can be distressing not only for the person experiencing it but also for their caregivers.
What is Sundowning
Causes of Sundown Syndrome
The exact cause of sundown syndrome is not fully understood, but several factors are believed to contribute to its onset:
Disruption of the Internal Body Clock: People with dementia often have a disrupted circadian rhythm, which can lead to confusion and agitation as night falls.
Environmental Factors: Dim lighting and shadows can confuse and frighten someone with dementia, exacerbating symptoms of sundowning.
Fatigue: As the day progresses, tiredness can set in, making it harder for individuals to manage their symptoms.
Psychological Factors: The onset of darkness can trigger fear and anxiety in some people, leading to agitation.
Symptoms of Sundown Syndrome
The symptoms of sundown syndrome can vary but typically include:
- Confusion and disorientation
- Anxiety, agitation, or aggression
- Pacing or wandering
- Mood swings
- Hallucinations or delusions
- Resistance to redirection or care
These symptoms can be particularly challenging for caregivers, as they often occur at a time when both the individual and the caregiver are tired.
When medication has an opposite response
Managing Sundown Syndrome
While there is no cure for sundown syndrome, there are strategies that can help manage its symptoms:
Maintain a Consistent Routine: Keeping a regular schedule for meals, bedtime, and activities can help reduce confusion and anxiety.
Create a Calming Environment: Reducing noise and clutter, and providing adequate lighting during the evening can help minimize agitation.
Encourage Physical Activity and Social Engagement: Regular exercise and social interactions can improve mood and help regulate sleep patterns.
Monitor Diet and Medications: Some foods and medications can exacerbate symptoms of sundowning. It’s important to consult with a healthcare provider to manage these factors effectively.
Provide Comfort and Reassurance: Offering a calm and reassuring presence can help ease anxiety and confusion during episodes of sundowning.
Impact on Caregivers
Caring for someone with sundown syndrome can be physically and emotionally taxing. Caregivers often report increased stress, sleep disturbances, and burnout. It's crucial for caregivers to seek support and respite care when needed to maintain their well-being.
Future Directions in Understanding and Managing Sundown Syndrome
Research into sundown syndrome is ongoing, with studies focusing on understanding its underlying causes and developing effective management strategies. There is also a growing emphasis on caregiver education and support, recognizing the vital role caregivers play in the management of this condition.
All of our guides, downloads, worksheets, Premium courses
Click Subscribe To Get Started.
Evening is a time to engage in quiet activities, such as:

Sundown syndrome is a complex condition that poses challenges for individuals with dementia and their caregivers. Understanding the nature of sundowning, its causes, and effective management strategies can significantly improve the quality of life for those affected. Ongoing research and support for caregivers will continue to play a crucial role in addressing this challenging aspect of dementia care.
What is a Paradoxical Effect with Medications?
The paradoxical effect of medications in the context of Sundown Syndrome, or sundowning in dementia patients, is a critical issue to consider. Typically, certain medications are prescribed to alleviate symptoms like agitation, anxiety, or sleep disturbances. However, paradoxically, these same medications can sometimes worsen the symptoms they are meant to treat or introduce new challenges.
Understanding the Paradoxical Effect
Increased Agitation and Confusion: Medications such as sedatives or antipsychotics, often used to calm patients, can lead to increased agitation or confusion in some individuals, particularly in those with dementia.
Heightened Sensitivity: Elderly patients, especially those with dementia, can be more sensitive to medications, leading to unexpected reactions, such as increased restlessness or aggression, instead of sedation or calmness.
Deterioration of Cognitive Functions: Certain medications might contribute to a further decline in cognitive functions, contrary to the intended purpose of stabilizing or improving these functions.
Management Strategies
Careful Medication Monitoring: It’s crucial for healthcare providers to closely monitor the effects of any medication prescribed to dementia patients, especially when starting a new medication or changing dosages.
Non-Pharmacological Approaches: Before resorting to pharmacological interventions, non-pharmacological strategies should be considered. These include environmental modifications, establishing routines, and using calming techniques.
Personalized Treatment Plans: Treatment for sundowning should be highly individualized, taking into account the patient’s history, current condition, and how they have previously reacted to certain medications.
Regular Reassessment: Regular reassessment of the patient’s medication regimen is vital to ensure that the benefits of a medication outweigh any adverse effects, including paradoxical reactions.
Conclusion
The paradoxical effects of medications in treating Sundown Syndrome highlight the need for a cautious, individualized approach to pharmacological management in dementia patients. Balancing medication benefits with potential risks is essential for effective and safe treatment of sundowning symptoms.
Update
Rexulti: A New Horizon in Treating Agitation in Alzheimer’s-Related Dementia
Rexulti (brexpiprazole) is an antipsychotic medication that has recently gained recognition for its use in treating agitation associated with dementia due to Alzheimer’s disease. This marks a significant development in the management of symptoms commonly associated with sundown syndrome in dementia patients.
Mechanism of Action and Uses
- Rexulti functions by altering the actions of serotonin and dopamine, two key neurotransmitters in the brain. This pharmacological action contributes to its effectiveness in managing certain psychiatric conditions.
- It is prescribed for treating major depressive disorder, schizophrenia, and specifically agitation associated with Alzheimer’s-related dementia.
FDA Approval and Significance
- Significantly, Rexulti is the first and only therapy to receive approval from the U.S. Food and Drug Administration (FDA) specifically for the treatment of agitation in patients with dementia due to Alzheimer’s disease. This approval underlines the medication's unique role in addressing this challenging aspect of dementia care.
Dosage and Administration
- The recommended starting dosage of Rexulti for treating agitation associated with Alzheimer’s dementia is 0.5 mg once daily for the first week. The dosage is then increased to 1 mg daily for the second week, and subsequently to 2 mg daily from the fifteenth day onwards.
- It is important to note that Rexulti should not be used as an “as needed” treatment for agitation but should be administered as part of a regular medication regimen.
Side Effects
- Common side effects reported during clinical trials for patients with dementia-related agitation include headaches, dizziness, urinary tract infections, nasopharyngitis, and sleep disturbances.
- As with any medication, it's crucial for caregivers and healthcare providers to monitor for any adverse effects and adjust the treatment plan accordingly.
In summary, Rexulti offers a new avenue for managing agitation associated with Alzheimer’s-related dementia, a symptom complex often seen in sundown syndrome. Its specific approval for this use highlights its potential effectiveness, although attention must be paid to dosing guidelines and potential side effects.
Our Resources section can help you find the information and tools that you need. We have courses, videos, checklists, guidebooks, cheat sheets, how-to guides and more.
You can get started by clicking on the link below. We know that taking care of a loved one is hard work, but with our help you can get the support that you need.
Click here to go to Resources Section now!
You might also like this article: