Cheyne Stokes Breathing: How Long Does It Last at End of Life?
Cheyne-Stokes breathing, a common breathing pattern near the end of life, can be distressing for caregivers. Learn what it is, how long it typically lasts, and how to provide comfort during this phase of the dying process in our detailed guide.

Cheyne-Stokes breathing is a pattern of breathing that occurs when a person’s respiration rate increases and decreases over a period of time. This type of breathing is commonly seen at the end of life and can be a sign of a serious medical condition.
Cheyne-Stokes respiration is an irregular breathing pattern associated with various medical conditions such as central sleep apnea, heart failure, and stroke. It is characterized by an alternating pattern of decreased breathing, known as apnea, followed by periods of deep, rapid breaths. Apnea is a temporary pause in breathing, usually lasting between five to ten seconds. This pattern typically repeats itself between five and twenty times throughout the course of the day. Understanding its underlying causes and potential treatments is crucial, as it can indicate serious health issues or the dying process, especially during sleep.
At the end of life, Cheyne-Stokes breathing can be a sign of an underlying medical condition or the body’s natural response to approaching death. It is often the result of low brain oxygen levels, which can be caused by a stroke, tumor, or other neurological issues. In addition, impaired respiratory system function due to COPD, heart failure, or other medical conditions can also contribute to the development of Cheyne-Stokes breathing.
It is important to note that not all cases of Cheyne-Stokes breathing indicate a life-threatening condition, but it is still essential to discuss any abnormal breathing patterns with a doctor. Left untreated, Cheyne-Stokes breathing can have profound complications at the end of life as it can cause fatigue, confusion, and disorientation. Therefore, it is important to understand the causes and risk factors associated with this condition, as well as the available treatment options.

Understanding Cheyne-Stokes Breathing
Definition and Characteristics
Cheyne-Stokes breathing is a type of abnormal breathing pattern characterized by cycles of slow, deep breathing followed by rapid, shallow breathing, and then a period of apnea or no breathing. This pattern is often seen in individuals with serious medical conditions, such as heart failure, stroke, or brain damage. Cheyne-Stokes breathing is a compensatory mechanism that helps regulate breathing and maintain oxygen levels in the blood. During these cycles, the body attempts to balance the levels of oxygen and carbon dioxide, which can become disrupted due to underlying health issues. This irregular breathing pattern can be distressing to observe, but it is a natural response of the body trying to cope with decreased oxygen levels.
Normal Breathing vs. Cheyne-Stokes Breathing: Key Differences
Normal breathing is a regular, rhythmic process that involves the contraction and relaxation of the diaphragm and other respiratory muscles. In contrast, Cheyne-Stokes breathing is an irregular pattern of breathing that is often accompanied by pauses in breathing. The key differences between normal breathing and Cheyne-Stokes breathing are:
- Breathing rate: Cheyne-Stokes breathing is characterized by a slow breathing rate, often less than 12 breaths per minute, followed by rapid breathing. This fluctuation in the rate is a stark contrast to the steady pace of normal breathing.
- Breathing depth: Cheyne-Stokes breathing involves deep, labored breathing, followed by shallow breathing. Normal breathing maintains a consistent depth, ensuring efficient gas exchange in the lungs.
- Apnea: Cheyne-Stokes breathing is often accompanied by periods of apnea or no breathing. These pauses can last for several seconds and are not present in normal breathing patterns.
Understanding these differences can help caregivers and family members recognize Cheyne-Stokes breathing and seek appropriate medical advice and support.
Causes of Cheyne-Stokes Breathing at End of Life
Cheyne-Stokes breathing is a pattern of breathing characterized by regular waxing and waning in the depth and rate of respiration. It typically appears during the end of life due to decreasing oxygen levels in the brain, often caused by a stroke, brain tumor, or other neurological issues. Monitoring vital signs, including blood pressure, is important as they might fluctuate or decrease near the end of life.
Impaired respiratory system function can also contribute to the development of this type of breathing. Factors like COPD, pulmonary embolism, or chronic bronchitis could cause Cheyne-Stokes breathing due to decreased lung capacity or accumulation of fluids in the lungs.
Other medical conditions may have an influence on end-of-life breathing patterns. These could include heart failure, kidney failure, metabolic imbalances, and drug overdose.
In some cases, Cheyne-Stokes breathing can be a sign of underlying diseases like pneumonia, sepsis, or acute respiratory distress syndrome (ARDS). All of these conditions may result in more rapid breathing or shallow breaths.
Cheyne-Stokes Breathing in the Dying Process
Relationship between Cheyne-Stokes Breathing and Death: A Sign of Impending Death
Cheyne-Stokes breathing is often seen in individuals who are nearing the end of life. This breathing pattern is a sign that the body is shutting down and that death is imminent. In the dying process, Cheyne-Stokes breathing is often accompanied by other signs and symptoms, such as:
- Noisy breathing: Also known as the “death rattle,” noisy breathing is a common symptom in the dying process. This occurs due to the accumulation of secretions in the throat and airways, which the individual can no longer clear effectively.
- Shallow breathing: As the body weakens, breathing becomes shallower and more labored. This is a natural progression as the body’s systems begin to slow down.
- Rapid breathing: In the final stages of life, breathing may become rapid and irregular. This can be a response to the body’s decreasing ability to maintain adequate oxygen levels.
- Apnea: Periods of apnea or no breathing are common in the dying process. These pauses can become longer and more frequent as death approaches.
Cheyne-Stokes breathing is a natural part of the dying process, and it is not typically painful or distressing for the individual. However, it can be upsetting for family members and caregivers. Providing emotional support and comfort during this time is essential. Simple measures such as playing soft music, ensuring a calm environment, and being present can make a significant difference in the comfort of the dying person. Understanding that Cheyne-Stokes breathing is a normal part of the dying process can help caregivers and family members cope with the emotional challenges they may face.

Treatment Options for Cheyne-Stokes Breathing at End of Life, Including Oxygen Therapy
When someone is nearing end of life, their body can be in a vulnerable state. As such, medical practitioners may use treatments to help ease their symptoms and discomfort. One such symptom that might be experienced is Cheyne-Stokes breathing. This can be addressed by a number of available medications and therapies.
Supplemental oxygen is one available medication for the treatment of Cheyne-Stokes breathing. Oxygen can help improve the level of oxygen in the blood, which can be especially helpful if someone is experiencing low oxygen levels due to a stroke, brain tumor, or other neurological issues. Oxygen therapy may be beneficial for some patients with low oxygen levels, but it is not universally effective. Medical staff may need to adjust its use based on the patient's comfort and response. In addition, bronchodilators are a class of drugs that can relax the muscles around the airways, making it easier to breathe.
Other treatments include administering sedatives and muscle relaxants to reduce restlessness and agitation, as well as pain relievers to manage any discomfort. All of these medications can be used in combination with supportive therapies, such as massage or music therapy, to create a more comforting environment and promote relaxation.
Anatomical Considerations
Cheyne-Stokes respirations are a pattern of respiration that is marked by alternating periods of shallow breathing and deep, rapid breaths. It can affect people of any age, but is particularly concerning near the end of life, as it can worsen a patient’s symptoms and even contribute to mortality. To better understand this phenomenon, it’s important to look at the anatomy behind it.
The respiratory system is responsible for bringing oxygen into the body and removing carbon dioxide. This is done through the regular contraction and relaxation of the diaphragm, intercostal muscles, and external intercostals. With Cheyne-Stokes respirations, these muscles become overly relaxed, resulting in alternating periods of deep, rapid respiration and shallow breathing. This can lead to decreased oxygen levels in the brain, which can be further worsened by a stroke, brain tumor, or other neurological issues.
Airway obstruction can also cause central apneas, or periods when a person stops breathing completely. Air sac abnormalities in the lungs can also have an impact on end-of-life breathing patterns. These abnormalities may include blockages due to thick secretions, fluid accumulation, or tumors.
It’s essential to understand the anatomy behind Cheyne-Stokes respirations in order to develop effective strategies for treating and preventing this condition. By recognizing the implications of decreasing brain oxygen levels and air sac abnormalities, healthcare practitioners can work to ensure that a patient’s respiratory and overall health are well-maintained during their end-of-life journey.
Risk Factors that Contribute to Cheyne-Stokes Breathing
When a person is approaching the end of their life, it can be distressing for them and their loved ones. One sign of nearing the end is Cheyne-Stokes breathing. This is a pattern of shallow breaths with periods of apnea (a temporary pause in breathing). Even though there is no exact cause of this type of breathing for those at end of life, there are certain lifestyle choices and medical conditions which can increase risk.
For example, smoking and drinking alcohol are both risk factors for developing Cheyne-Stokes breathing. Smoking can damage the lungs over time, making it difficult for them to effectively take in oxygen. Alcohol consumption has also been linked to respiratory difficulty. Depending on the severity of the condition, medications such as bronchodilators and supplemental oxygen may be needed to help manage symptoms. It is important for caregivers or family members to report any changes in these vital signs to the hospice nurse, who can provide appropriate support and guidance.
In addition to lifestyle choices, some medical conditions can cause or worsen Cheyne-Stokes breathing. If a person is diagnosed with a stroke, brain tumor, or other neurological issues, their brain oxygen levels can decrease significantly. This can cause their breathing to become irregular and shallow. Impaired respiratory system function caused by asthma, COPD (Chronic Obstructive Pulmonary Disease), or cystic fibrosis may also trigger Cheyne-Stokes breathing at end of life.
Address Possible Complications
One of the most concerning aspects about Cheyne-Stokes breathing at the end of life is its tendency to complicate existing medical conditions. Patients with secundum atrial fibrillation or semi-lateral end-stage renal disease may experience particularly difficulty during this time as their health deteriorates.
Secundum atrial fibrillation, or AFib, occurs when the heart's electrical signals become so chaotic that the atrium begins pumping in an irregular way. This causes poor circulation, breathlessness, and lightheadedness. It can also cause arrhythmias, which can make breathing even more difficult. People who develop AFib close to death may experience an increased risk for Cheyne-Stokes breathing.
Semi-lateral end-stage renal disease, or ESRD, is a complex condition where the kidneys fail to properly filter toxins from the body. When someone is close to death, their failing kidneys can cause a buildup of toxic fluids in the lungs, further exacerbating symptoms of Cheyne-Stokes breathing.
Both of these conditions can significantly complicate the patient's prognosis and often require treatment. It is important to stay aware of any potential medical complicating factors when a patient is close to death, as they may affect the course of their Cheyne-Stokes breathing.
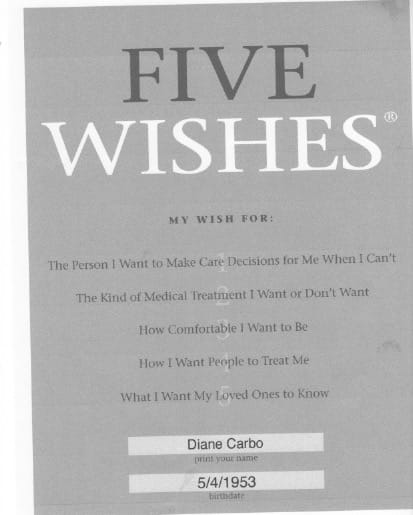
Outlining End-of-Life Care
Making sure your loved one is comfortable and has access to end-of-life care is essential during their final days. There are multiple points of care you can focus on for the best comfort and aid. Nutrition, environment, and emotional support should be your three main points of focus.
Nutrition
Nutrition plays a role in overall health, and that includes end-of-life care. Eating nutritious meals is an important part of providing comfort and can help the patient have more energy and better withstand treatment. Make sure to find out what foods the patient likes and provide those. Soft, easy to digest foods might be easier if it's difficult to eat larger meals. You can also check with the patient's doctor or nutritionist for advice.
Environment
Creating a peaceful and comfortable environment is vital. Keeping the room at a comfortable temperature, providing pillows and blankets, and using white noise machines to create a relaxing atmosphere are all great ways to make sure your loved one is as comfortable as possible.
Emotional Support
Supporting your loved one during their end-of-life journey can be incredibly challenging. Making sure you are present and listening to any of their concerns can help greatly. Having conversations with them and reminding them of the positive things in their life can also be very beneficial. Simply being there and giving them your love can go a long way.
During this delicate time, keeping your loved one comfortable and taken care of is important. Maintaining nutrition, creating a peaceful environment, and providing emotional support are just some of the many ways you can provide comfort and aid while they are in their last days.
Stress Prevention Strategies for Reducing Cheyne-Stokes Breathing
Cheyne-Stokes breathing is a type of breathing pattern that can become present at the end of life. It is important to understand possible stress prevention strategies in order to reduce the severity and prevalence of this condition. By implementing the following tips, those at risk of developing Cheyne-Stokes breathing may be able to reduce its chances.
- Avoid smoking and other prohibited substances.
- Manage stress levels by getting plenty of rest and exercising regularly.
- Eat a healthy diet and stay hydrated.
- Make sure to take medications as prescribed by the doctor.
- Keep the environment quiet and comfortable.
- Receive regular medical check-ups to monitor any potential health issues.
It is also important to be aware of early signs and symptoms of Cheyne-Stokes breathing so that you can get treatment as soon as possible. These symptoms include shallow, irregular breathing, pauses between breaths, and excessive yawning. If these symptoms appear, contact your doctor right away to begin discussing possible treatments.
By keeping these strategies in mind, those at risk of developing Cheyne-Stokes breathing may be able to reduce their chances. As always, it is important to seek advice from a healthcare provider before making any changes to lifestyle or attempting to treat any medical condition.
Ascertaining the Prognosis
Cheyne-Stokes breathing at end of life can have a variety of effects on the length of time a patient may be affected, and other medical complications may also affect their prognosis. It is widely thinking that this type of breathing could be linked to mortality, so it's important to understand the potential implications.
The exact length of time a patient may be affected by this condition depends on the cause of the Cheyne-Stokes breathing and the other medical conditions present in the patient. Generally, patients will experience a decrease in breathing rate over several days as they approach death. Additionally, other medical complications such as heart failure or chronic obstructive pulmonary disease can worsen the prognosis.
The potential link between Cheyne-Stokes breathing and mortality is still being studied. While some studies have suggested that the presence of this type of breathing can be a predictor of death, other studies have not found the same correlation. Research suggests that the severity and duration of the condition are important indicators of mortality.
It's important to note that Cheyne-Stokes breathing at end of life is a normal part of the dying process. However, as it can be uncomfortable and indicate additional medical issues, it is important to understand the possible implications of this condition.
Cheyne-Stokes breathing is a type of abnormal breathing pattern that can occur at the end of life. It is characterized by alternating periods of shallow and deep breaths, and can be accompanied by pauses in the breathing cycle. This troubling symptom can be caused by a variety of conditions, including a stroke or brain tumor, impaired respiratory system function, and other medical conditions. Treatment options, such as supplemental oxygen or bronchodilators, are available to help ease the patient's symptoms.
It is important to understand the anatomical considerations, risk factors, and possible complications associated with Cheyne-Stokes breathing at end of life, as they may influence the prognosis and treatment options. Additionally, proper end-of-life care, such as staying nourished, avoiding stress, and providing emotional support, is essential for maintaining quality of life in these later stages.
The good news is that there are strategies to help reduce the severity and prevalence of Cheyne-Stokes breathing. With proper medical care and support, patients can find some comfort and assurance during this time. If you are looking for additional resources on this topic, please consult your doctor or reach out to local support groups.
You might also like this article: